How to Appeal Medicare Coverage Decisions
If you’re covered by Medicare, whether under Original Medicare, a Medicare Advantage plan, or a Medicare drug plan, you have the right to challenge decisions when coverage or payment for a service, drug, or item is denied or reduced.
Below is how you can appeal such decisions, step by step, so you know what to do if/when it happens.
When You Can Appeal
You can appeal a decision whenever Medicare or your plan makes a coverage choice you believe is incorrect. For example, if a service, supply, item, or drug is denied, reduced, or stopped, you have the right to challenge that outcome. Many beneficiaries appeal when Medicare refuses to pay for a service they already received, when a plan says a treatment is not medically necessary, or when the amount they are asked to pay seems too high. You can also appeal if a Part D drug plan places limits on a medication through its safety or monitoring programs and you feel the restriction is not appropriate. In every one of these situations, beneficiaries are allowed to ask for a formal review.
How the Appeals Process Works, Different Paths for Different Coverage Types
The exact steps you take depend on what type of Medicare coverage you have: Original Medicare or a Medicare plan (like Medicare Advantage or a drug plan).
Original Medicare (Fee-for-Service)
If you have Original Medicare and you receive a notice (called a Medicare Summary Notice or MSN) that denies or reduces payment for a service or item, here is how to appeal:
-
Level 1 – Redetermination: You (or your representative) request a redetermination from the contractor that handles Medicare claims. You must file within 120 days of receiving the MSN.
-
If the redetermination is unfavorable, you can move to a Level 2 – Reconsideration. This involves an independent contractor (not the same one who made the original denial) reviewing your case. Typically you must request reconsideration within 180 days of receiving the redetermination decision.
-
If still denied, you can request a hearing before an Administrative Law Judge (ALJ) through the Office of Medicare Hearings and Appeals (OMHA). That is Level 3.
-
After the ALJ: Level 4 is a review by the Medicare Appeals Council. If that decision is still unfavorable, you may be able to take your appeal to Federal District Court (Level 5) — but only if the amount in dispute meets a certain minimum threshold.
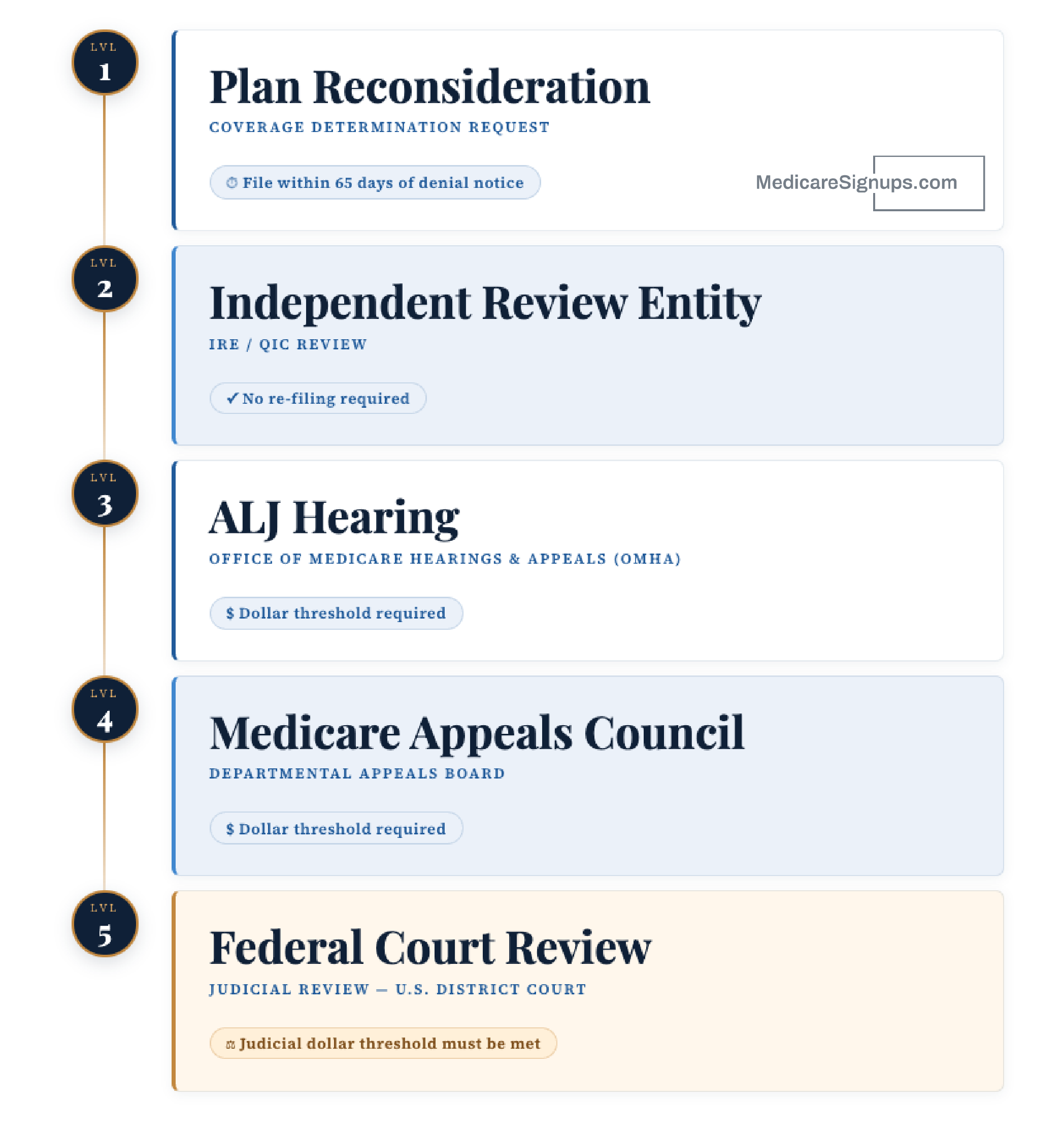
Medicare Advantage (Part C) or Medicare Drug Plans (Part D)
If you are enrolled in a Medicare Advantage or Part D drug plan, the appeal process is somewhat different.
-
Level 1 – Plan Reconsideration (Health Plan Reconsideration / Coverage Determination Request): If your plan denies (or reduces) coverage, you (or your doctor) must request reconsideration. This must be done within 65 days of receiving the denial notice.
-
If the plan upholds its decision, your appeal moves to Level 2 – Independent Review Entity (IRE / QIC) Review. The plan sends your case automatically; you do not need to re-file.
-
If still denied, you may request a hearing before an ALJ (through OMHA) — Level 3.
-
Then Level 4 – Medicare Appeals Council can review the ALJ’s decision.
-
Finally, in some cases you may go to Federal Court (Level 5) — but again, only if your case meets the dollar-amount requirement for judicial review.
If waiting for standard appeals would endanger your health, you (or your doctor) can request an expedited appeal. For example, for a pre-service request or a Part B drug you may get a decision in within 72 hours.
What You Should Do Before You File
Before starting an appeal, it is helpful to gather as much information as possible. Begin by reading your denial notice or your Medicare Summary Notice carefully so you understand the reason Medicare or your plan made its decision. These notices also include instructions that explain where and how to submit your appeal. Many beneficiaries ask their doctor or medical provider to supply reports, visit notes, test results, or statements that explain why the service or item was medically necessary. If you want a family member, friend, or advocate to help you through the process, make sure Medicare or your plan has the needed paperwork that allows that person to speak on your behalf. Preparing these details ahead of time often creates a clearer and stronger appeal.
What to Expect: Timeline & What If You Still Disagree
-
For Original Medicare, you generally must file a redetermination within 120 days of the MSN.
-
For Medicare Advantage or drug plan denials, you must request reconsideration within 65 days after you get the denial notice.
-
If you qualify for an expedited review (e.g., due to serious health risk), the plan must act within 72 hours.
-
If you reach the ALJ hearing level, expect the process to take longer, but you will have the chance to present your case in person or by phone/video.
-
If after all levels you still disagree and your case meets the financial threshold, you may be able to request a review by a Federal District Court.
What to Do If the Denial is About a Drug or a Treatment You Need Immediately
If the denial involves a prescription or treatment that you need right away, do not wait to start the appeal process. You may be eligible for an expedited review, which is a faster type of appeal used when a delay could harm your health or lower your chance of recovery. Your doctor can support your request by explaining why the treatment is urgently needed. When an expedited appeal is approved, the plan must review your case within a short period of time, often within 72 hours. Acting quickly and providing medical details that show why the delay would be risky gives you the best chance of receiving a fast decision.
When It Might Be Worth Getting Help
Once you reach the formal hearing levels (especially ALJ hearings or beyond), the process gets more complicated. You may want help from:
-
A lawyer familiar with Medicare law
-
A trusted representative (family member, patient advocate)
-
Local assistance programs (your state’s health insurance assistance program, senior-advocacy groups)
Even if not required, having help can improve your chances of a favorable outcome.
Final Thoughts
If Medicare or your plan denies coverage or payment for a service, drug or supply you believe you’re entitled to, don’t assume that’s the end of the road. You have rights; the right to appeal, the right to present extra information, the right to a hearing, and even the right to take your case to federal court under certain circumstances.
Take action early… appeals have strict deadlines. Gather documentation, ask your doctor for support, and follow the instructions on your denial notice carefully.
Appealing can feel complicated, but for many beneficiaries it is the difference between getting the care they need or paying out of pocket.